
Diabetic Foot Problems
Diabetic Foot Problems
Diabetic Foot Ulcer
Some people with diabetes develop foot ulcers.
What is a foot ulcer?
A foot ulcer is where an area of skin in the foot has broken down and the underlying tissue is visible. This can be even after a mild injury such as stepping on a small stone or because of pressure damage from tight fitting shoes.
Why are people with diabetes prone to foot ulcers?
Foot ulcers are more common in diabetes because one or both of the following problems which occur in some people with diabetes:
Reduced skin sensation in the feet
Diabetes is a disease characterised by increase in blood sugar levels. This leads to deposition of sugar in the tissues damaging the nerves. This is called as called peripheral neuropathy of diabetes. The nerves that take messages of sensation and pain from the feet are commonly affected. Additionally, numbness in the feet makes them prone to injury. Also, if you cannot feel pain from the foot, you do not protect small wounds by not walking on them. Therefore, they can quickly become worse and develop into ulcers.
Narrowing of arteries (blood vessels) going to the feet
If you have diabetes you have an increased risk of developing narrowing of the arteries (peripheral vascular disease). The arteries in the legs are quite commonly affected. This can cause a reduced blood supply (poor circulation) to the feet. Therefore, if you get a minor cut or injury, it may take longer to heal and be prone to becoming worse and developing into an ulcer especially when neuropathy is also there.

What increases the risk of developing foot ulcers?
1. Numbness in the feet due to neuropathy
2. Poor circulation due to narrowing of arteries
3. If you have had a foot ulcer in the past
4. If you have other complications of diabetes, such as kidney or eye problems
5. If your feet are more prone to minor cuts, grazes, corns or calluses which can occur
6. Ulcers are more common in people who smoke and those with poorly controlled diabetes
Are foot ulcers serious?
Foot ulcers if not treated can cause deep infection; gangrene and can rarely land up in amputation of leg. Adequate treatment by a foot specialist and good blood sugar control is necessary to prevent such complications.
What can I do to help prevent foot ulcers?
1. Have your feet regularly examined
Most people with diabetes are reviewed at least once a year by a doctor and other health professionals.
2. Treatment of diabetes and other health risk factors
As a rule, the better the control of your diabetes, the less likely you are to develop complications such as foot ulcers.
3. Self Foot care
Research has shown that people with diabetes who take good care of their feet and protect their feet from injury, are much less likely to develop foot ulcers.
What if I develop a foot ulcer?
You should tell your doctor about it. Most of the ulcers will heal with regular dressings and or if needed contact cast treatment. In some cases, the ulcer becomes worse, badly infected and does not heal. In these cases surgery is needed to control the infection. Sometimes the ulcer is not due to lack of circulation or numbness and infection. In such cases it is usually because of the bone pressure and a bone prominence under the arch of the foot. These ulcers can become very large and must be treated by excision of prominent bone.
Diabetic heel ulcer Diabetic heel ulcer after treatment
Picture on the left showing diabetic heel ulcers. Note the healing with good diabetic control and regular treatment
Charcot Foot or Charcot Arthropathy of Foot
Charcot’s foot is a complication of diabetes that almost always occurs in those with peripheral neuropathy (nerve damage). When neuropathy is present, the bones and joints in the foot do not have normal protective sensations like pain. Because of this patients with diabetes can overload their feet and can develop stress fractures in the bones of the feet even though they do not feel any pain. As patient do not have pain, they continue to walk overloading their feet thereby converting small stress fractures into complete fractures.
Another way to explain this is that imagine if you continue to drive your car with a punctured flat tyre, the pressure from the steel rim will cut through the tyre and completely destroy it.
As the fractured foot is loaded fractures get displaced leading to development of severe deformities.
How do I know if I have Charcot Foot?
It is often difficult to make diagnosis of Charcot foot until unless the foot deformity develops. However the affected foot is often swollen, red and warmer as compared to other foot. A deformity gradually develops as fractures displaces and joint dislocates due to disintegration of ligaments.
Diabetic Charcot foot with midfoot break Diabetic Charcot foot with midfoot ulcer
Most common deformity is midfoot break leading to rocker bottom deformity. As a result of deformity ulcers can develop over the newly developed bony prominences.
What is the treatment for Charcots Foot?
The prevention of further joint destruction and foot deformity is the primary aim in treatment of Charcot’s foot. Rest and stabilization of the foot is a key. Most cases should be put in a total contact cast to relieve pressure and to prevent further deformity. These need to be replaced periodically until there is no temperature difference between the two feet. This can take up to 6-9 months. Care needs to be taken of the other foot to prevent problems developing.
A drug (bisphosphonates)have been shown to be useful as an adjunct in the management of Charcot’s foot. After the Charcot foot has healed specialized footwear and foot orthoses may be needed to prevent it happening again (this may depend on the extent of deformity).
If treatment was not started early enough and/or the foot is deformed, the possibility of an ulcer developing is high. Prevention with footwear and foot orthoses is then very important.
If the deformity is severe or ulcer recurrence is a problem, surgery can be used to reshape the deformity. This may vary from a simple removal of a bony prominence to a fusion of joints to realign the foot.
Diabetic Charcot foot X-ray showing deformity before surgery Correction of deformity with surgery
X-ray showing deformity of foot secondary to diabetic charcot foot. This young patient was having problems with recurrent ulcer. He underwent correction of deformity by midfoot fusion
ALSO READ


How To Choose The Ideal Paper Writing Service
Posted On 24 May 2023
When you use a paper writing service, then you are picking a company that's devoted to your needs. They are…
APA Live Chat – The Way I Could Write My Paper?
Posted On 8 May 2023
If you've got a big test coming up and you need to have it done on time, and then you…
How to Write My Paper Cheaply
Posted On 7 May 2023
There are many ways to compose my paper inexpensively. In fact, some approaches can actually save money for the writer.…
Posted On 4 May 2023
Have Fun and Enjoy a Fun Way to Enjoy your time at home by playing free slots at the casino…
How to Write My Essay About Writing Sample Papers
Posted On 23 Apr 2023
Are you worried about how to write my own article? I understand, it's somewhat intimidating when you first begin learning…
College Application Essay Writing Service Voucher Reddit.com
Posted On 12 Apr 2023
This will suggest having a apparent being familiar with of the supply material or the subject and sticking shut to…
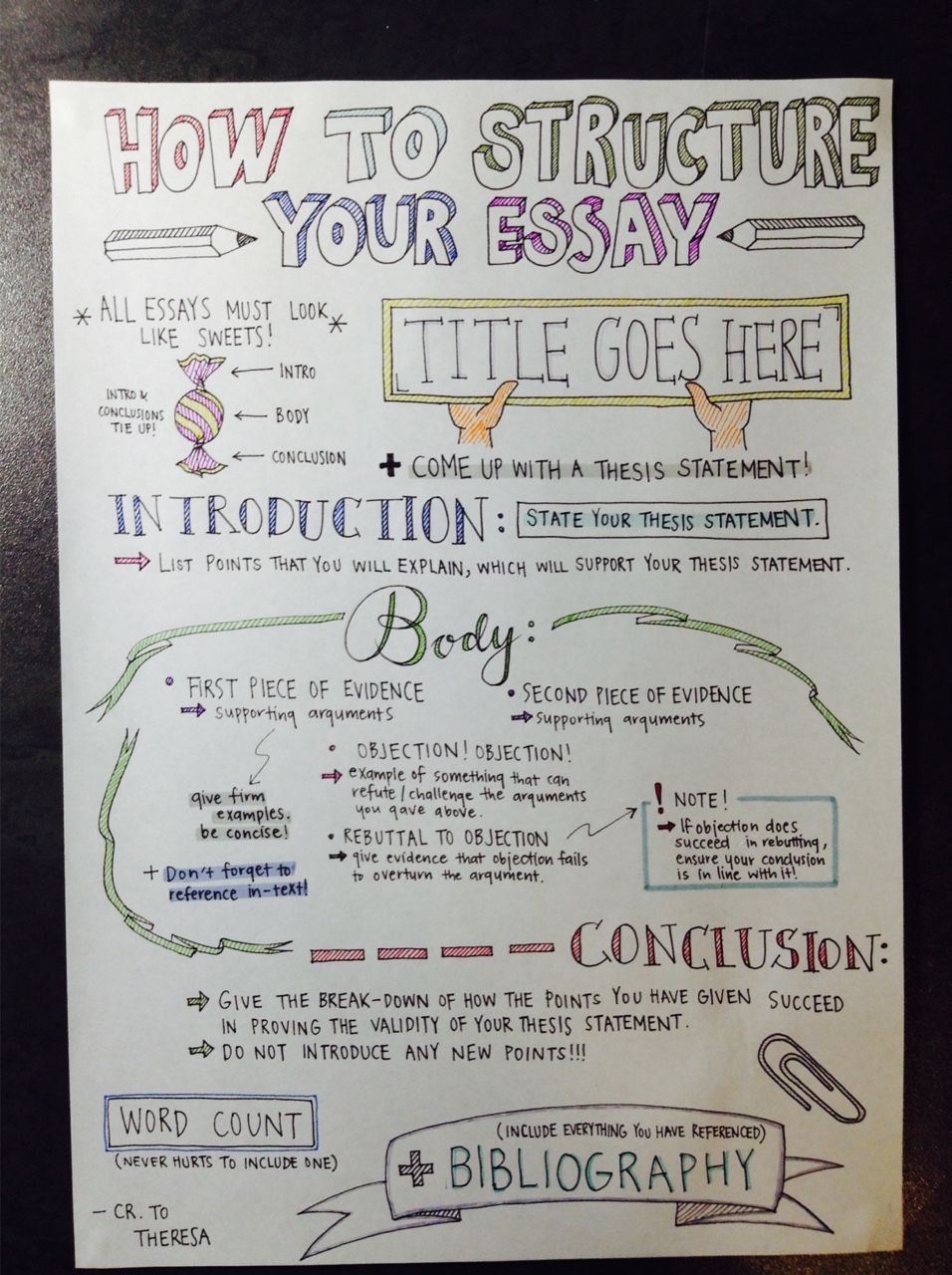
Quality Custom Essay Writing Service Reddit.com
Posted On 12 Apr 2023
Many universities present distinctive deals with savings which you could uncover fascinating. This way you will hardly ever free the…
Reddit Custom Essay Writing Service For Cheap
Posted On 12 Apr 2023
The Looming Questions: Will the reserve be a accomplishment or not? How considerably would this maximize your composing money? Now,…
Reddit Essay Writing Service Atlanta Ga
Posted On 11 Apr 2023
Pretty much as vital as firm any time you are producing essays, is concept generation. Nothing at all will kill…
Reddit.com Persuasive Essay Writing Service Online
Posted On 11 Apr 2023
As aspect of the organizing for faculty admissions, a timeline ought to be established in progress. Consequently, your site visitors…